Cataract Surgery
What is Cataract?
Cataract is a condition which partially or completely reduces the transparency of the lens in your eye, ultimately making you unable to read and to see the world around you. In cataract, your lens turns white in color and becomes opaque, from being previously color less and transparent. This can happen in one eye or both, though not necessarily at the same time.
Who gets Cataract?
Cataracts form as you grow old. Cataracts occur in people above the age of 50 and more often in people older than 60 years. Apart from age, cataract can also occur due to injury; or due to family history. You may also develop cataract if you are on long-term medications like steroids (including inhaled formulations) as well as certain medications for treatment of hypertension.
What are the indicators of cataract?
When you have a developing cataract, you will find it difficult to look at bright light which will dazzle, making it difficult to see. This effect is called Glare. You could also see “halo’s” around lights, or you may also have blurred vision.
Following are the common indicators of the presence of cataract Though, not all may occur together.
- Clouded, blurred or dim vision
- Increasing difficulty with vision at night
- Sensitivity to light and glare
- Seeing “halos” around lights
- Frequent changes in spectacles or contact lens prescription
- Fading or yellowing of colors
- Double vision in a single eye
How is Cataract treated?
Surgery is not always the first recommendation. If detected early, the doctor may prescribe spectacles or contact lens to improve your vision. As long as cataract doesn’t interfere with your everyday activities, you may not need surgery. But, if cataract has spread in the lens, enough to seriously impact your sight and your daily routine, the doctor may consider cataract surgery. If you have cataract in both eyes, the doctor will treat one eye first, and then the second eye several days Iater. This allows time for the first eye to heal.
What is cataract Surgery?
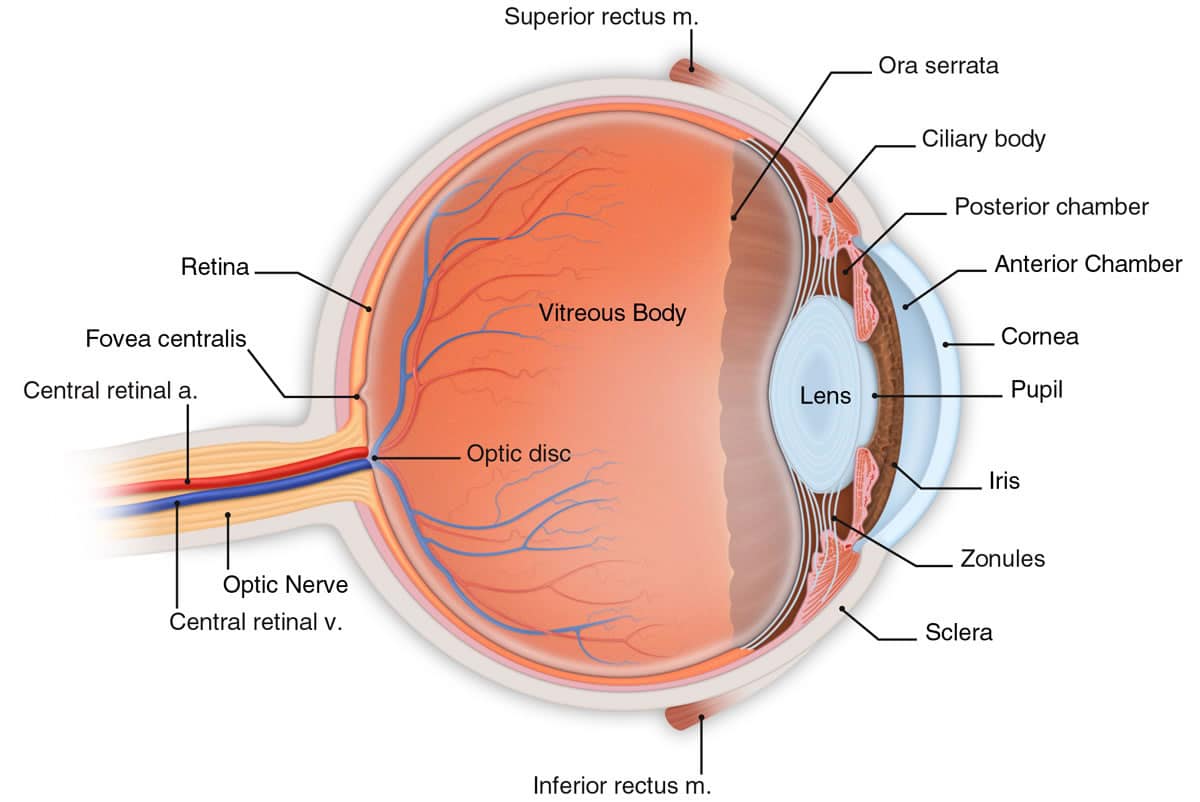
To understand what happens in cataract surgery, let’s look at the lens itself and how it is constructed. The human eye lens is made of protein fibers and water, with the fibers arranged in a pattern that allows light to pass through. In the normal eye the lens is clear and transparent. The lens has 3 layers – an outer Capsule which is like a “tough shell”, wrapped around the lens. Just under the Capsule is the soft lens Cortex, which contains cells that are active and continue to grow and divide. The Cortex covers the inner core or the Nucleus. This core becomes denser and harder as a person ages.
What Kind of surgery choices cam a cataract patient have?
There are three cataract surgery procedures:
lntracapsular cataract extraction (ICCE), Extracapular cataract extraction (ECCE) and Phacoemulsification (Phaco). ICCE is an outdated procedure and is no longer used, or performed very rarely.
What is ECCE ?
ECCE is also an old technique. In ECCE, the only the cataract-affected lens is removed, without removing the parts that hold the lens in place. After ECCE, you may have to use spectacles to further correct your eyes for sharper vision. Cataract surgeons in India have pioneered another technique called Small Incision Cataract Surgery (SICS). The benefits of SICS are, considerably shortened surgical time, quicker recovery, fewer post-operative complications and finally, lower cost than Phacoemulsification. Ask your doctor about SICS.

Contact Lenses
These are an efficient alternative to spectacles. Also, they give a better quality of vision. Many different types of materials are available with us. Many different regimes of wear are prescribed according to the patient’s needs. Strong prescriptions of contact lenses, unlike the spectacles, do not cause distortions.
Corneal Treatment
Corneal disease affects a transparent layer that shields your eyes from bacteria and debris. This condition may develop when you become injured or an infection occurs. Genetic traits can also trigger it. The symptoms range from light sensitivity to severe pain. Like many diseases, this medical problem comes in numerous varieties. The best solution differs depending on the specific type of corneal disease.
Neuro Opthamology
Neuro Ophthalmology is a specialty that concentrates on the neurological problems related to the eye. Like we all know, the human eye captures the visuals it sees and transmits to the brain to be resolved as images. It is the optic nerve that transmits these visual stimuli and a dysfunction of this entity might cause visual impairment and could even lead to irreparable damage.
COMMON SIGNS
- Reduced visual activity all of a sudden
- Double vision and headaches A less reactive pupil (pupil is the central part of eyeball that allows light to pass through)
- Impairment of colour vision (especially inability to identify red & green colours)
- Difficulty in seeing light (Photophobia)
- Visual Field Defects (visibility coverage)
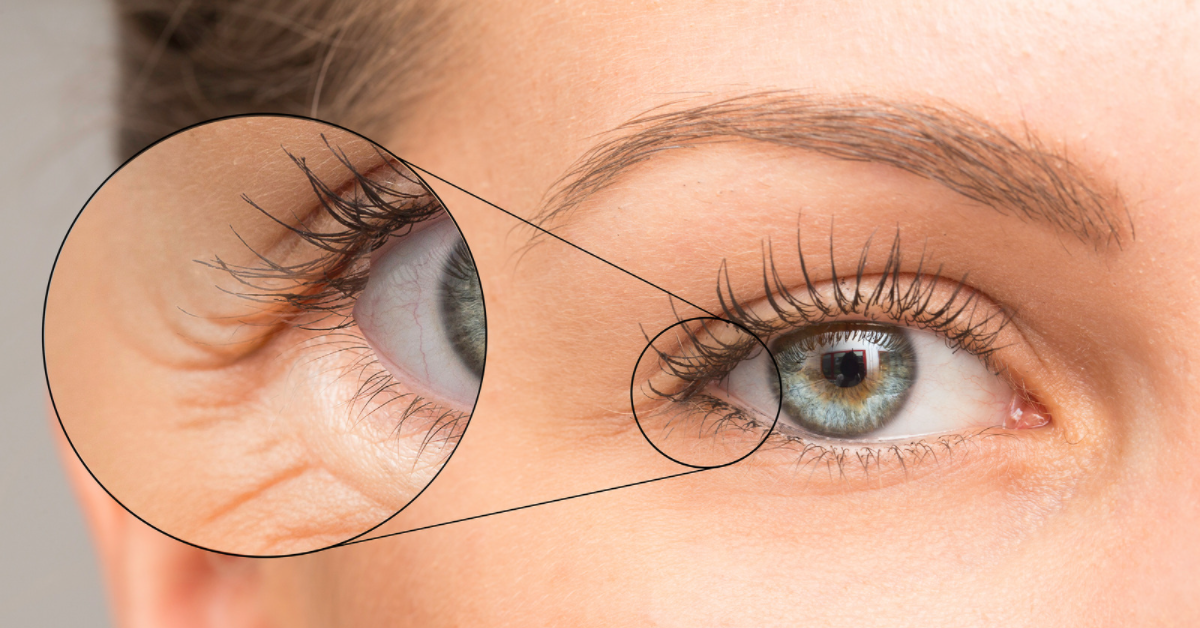
Oculoplastic Treatment
A specialized field in ophthalmology for cosmetic and non cosmetic treatments around the eyes and face.
Who provides Oculo-Facial Plasty services?
A trained oculo- facial plastic surgeon.
Which areas of the body are addressed?
- Forehead, Eyebrows, Eyelids, Lashes, Lacrimal (Tear passage), Socket (Eye cavity), Orbit (Bones around eyes), Eyeball, Cheeks.
- When should I see Dr. Goel?
Non-Cosmetic:
* Watering
* Itchy and red eyes
* Swelling, mass on eyelids/face
* Big/Small/Bulging eyes
* Thyroid
* Lid/ face injuries/fractures
* Eye/Face spasms/ twitching
* Painful blind eyes
* Infection on lids and face
* Tumors, malignancy
* In-turning/ Out-turning of lids
Cosmetic:
* Facial aging
* Skin issues
* Wrinkles/ lines
* Lumps, Bumps, Cysts
* Eye bags
* Droopy lids
* Puffiness of eyes
* Lost eye, Artificial eye
* Scars
* Dark circles
* Hollowness under eyes
Treatments:
* Ptosis correction
* Blepharoplasty
* Brow lift
* Botox and Fillers
* Skin care
* Scar revision
* Entropion correction
* Ectropion correction
DCR
* Trauma, injuries
* Lash procedures
* Removal of eye
* Facial paralysis treatment
* Socket reconstruction
* Orbit surgeries
* Reconstructions
Squint & Neuro-Ophthalmology Treatment
Cataract surgery is performed to treat cataracts. Cataracts can cause blurry vision and increase the glare from lights. If a cataract makes it difficult for you to carry out your normal activities, your doctor may suggest cataract surgery. When a cataract interferes with the treatment of another eye problem, cataract surgery may be recommended.
For example, doctors may recommend cataract surgery if a cataract makes it difficult for your eye doctor to examine the back of your eye to monitor or treat other eye problems, such as age-related macular degeneration or diabetic retinopathy. In most cases, waiting to have cataract surgery won't harm your eye, so you have time to consider your options. If your vision is still quite good, you may not need cataract surgery for many years, if ever.
When considering cataract surgery, keep these questions in mind: Can you see to safely do your job and to drive? Do you have problems reading or watching television? Is it difficult to cook, shop, do yardwork, climb stairs or take medications? Do vision problems affect your level of independence? Do bright lights make it more difficult to see?
Cornea Transplant Surgery
Cataract surgery is performed to treat cataracts. Cataracts can cause blurry vision and increase the glare from lights. If a cataract makes it difficult for you to carry out your normal activities, your doctor may suggest cataract surgery. When a cataract interferes with the treatment of another eye problem, cataract surgery may be recommended.
For example, doctors may recommend cataract surgery if a cataract makes it difficult for your eye doctor to examine the back of your eye to monitor or treat other eye problems, such as age-related macular degeneration or diabetic retinopathy. In most cases, waiting to have cataract surgery won't harm your eye, so you have time to consider your options. If your vision is still quite good, you may not need cataract surgery for many years, if ever.
When considering cataract surgery, keep these questions in mind: Can you see to safely do your job and to drive? Do you have problems reading or watching television? Is it difficult to cook, shop, do yardwork, climb stairs or take medications? Do vision problems affect your level of independence? Do bright lights make it more difficult to see?
Vitreoretinal Disease
Retina is the innermost photosensitive layer of the eye. It is connected to the brain via the optic nerve. It is located at the back of the eye. It is on this layer that an image seen by the eye is formed, which is converted to nerve signals and transferred to the brain.
The Retina Department at Swarup Eye Centre deals with the management of AMD, Diabetic retinopathy, Retinal detachment, Infections, Trauma & various other retinal disorders.
A highly trained team of surgeons combined with the effective use of latest diagnostic tools (FFA, ICG, B Scan, UBM, OCT) makes this department a major referral center for Vitreoretinal services.
AGE RELATED MACULAR DEGENERATION (AMD)
AGE RELATED MACULAR DEGENERATION(AMD)
The macula is the part of the retina that is responsible for your central vision, allowing you to see fine details clearly. Many older people develop macular degeneration as part of the body’s natural aging process. This is called age-related macular degeneration (AMD).
With macular degeneration, you may have symptoms such as blurred vision, dark areas or distortion in your central vision, and some times, permanent loss of your central vision. The peripheral vision is usually spared. Early symptoms are loss of clarity while reading and distortion of objects. With advanced macular degeneration you may fail to recognize a person’s face.
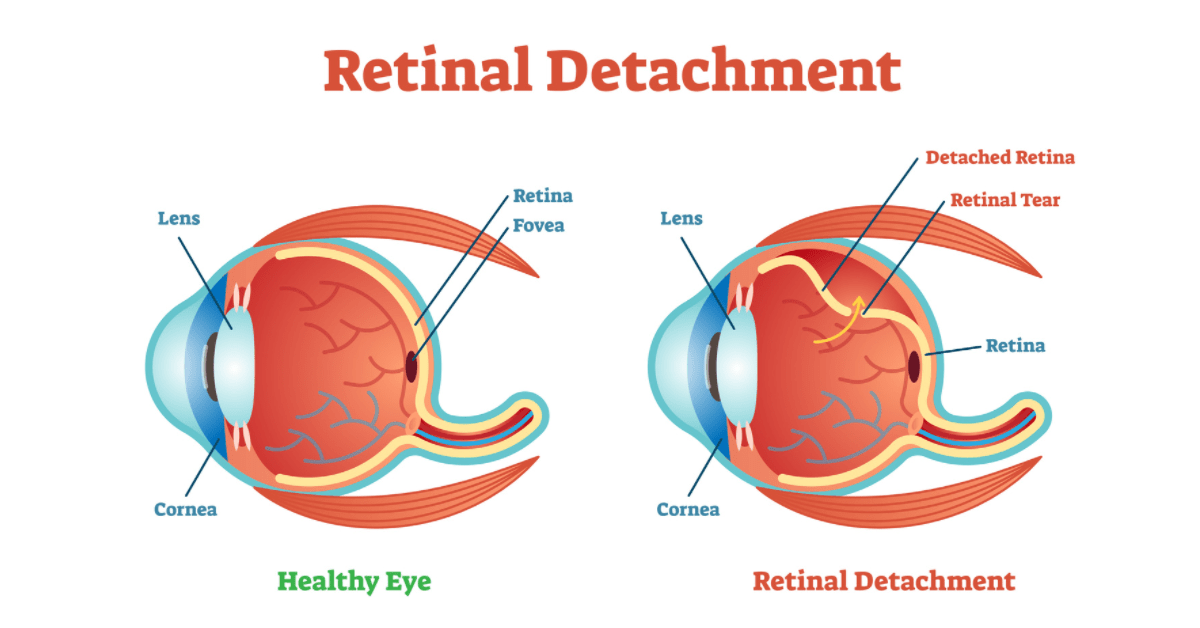
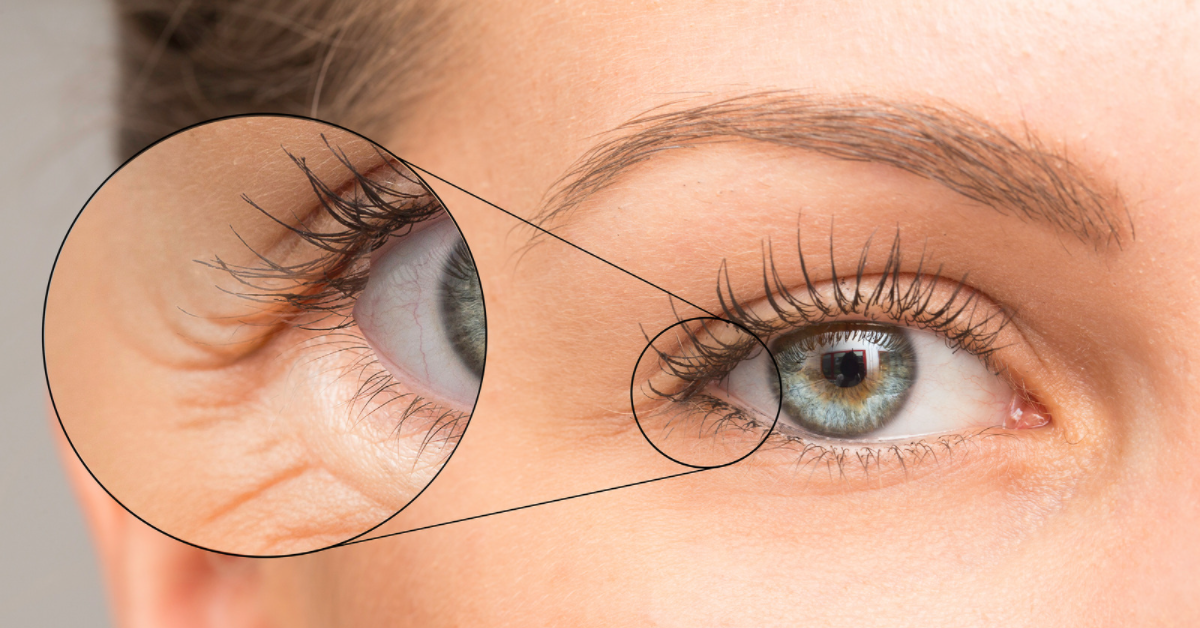
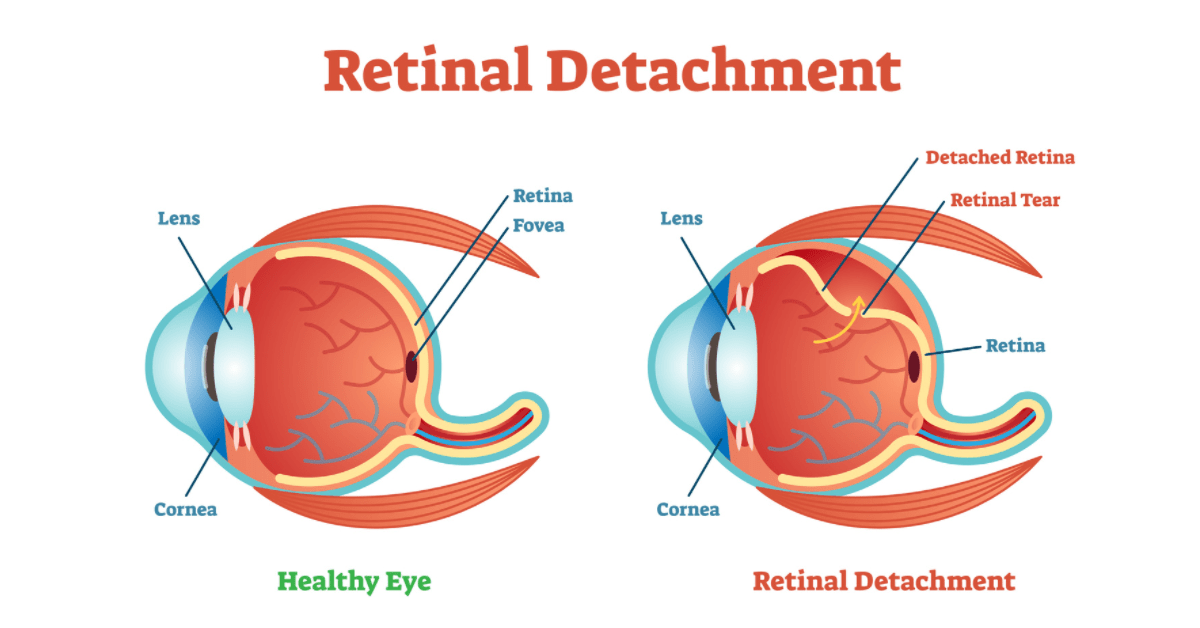
RETINAL DETACHMENT
The retina is the light-sensitive layer of tissue that lines the inside of the eye and sends visual messages through the optic nerve to the brain. When the retina detaches, it is lifted or pulled from its normal position. If not promptly treated, retinal detachment can cause permanent vision loss.
A retinal detachment can occur at any age, but it is more common in people over 40 years. It affects men more than women.
There are certain key symptoms of Retinal Detachment such as 1. Floaters, which are little ‘cobwebs’ or specks that float in your field of vision. 2. Sudden blurry vision 3. Flashes of light 4. An area of sudden dark vision.
Floaters are a common symptom in otherwise normal individuals. However if these are accompanied by persistent flashes, they could be symptoms of a retinal tear or detachment.
Swarup Eye Centre has state of the art and latest surgical equipment to deal with Retinal Detachment. Vitrectomy surgery is performed on patients with Retinal Detachment. Micro incision and sutureless (23/25 gauge) vitrectomy(MIVS) is performed using the Stellaris PC machine.
The advantages of this surgery are the absence of stitches in the eye; hence the post-operative recovery is faster.
Diabetic Eye Care
What is Diabetic Retinopathy?
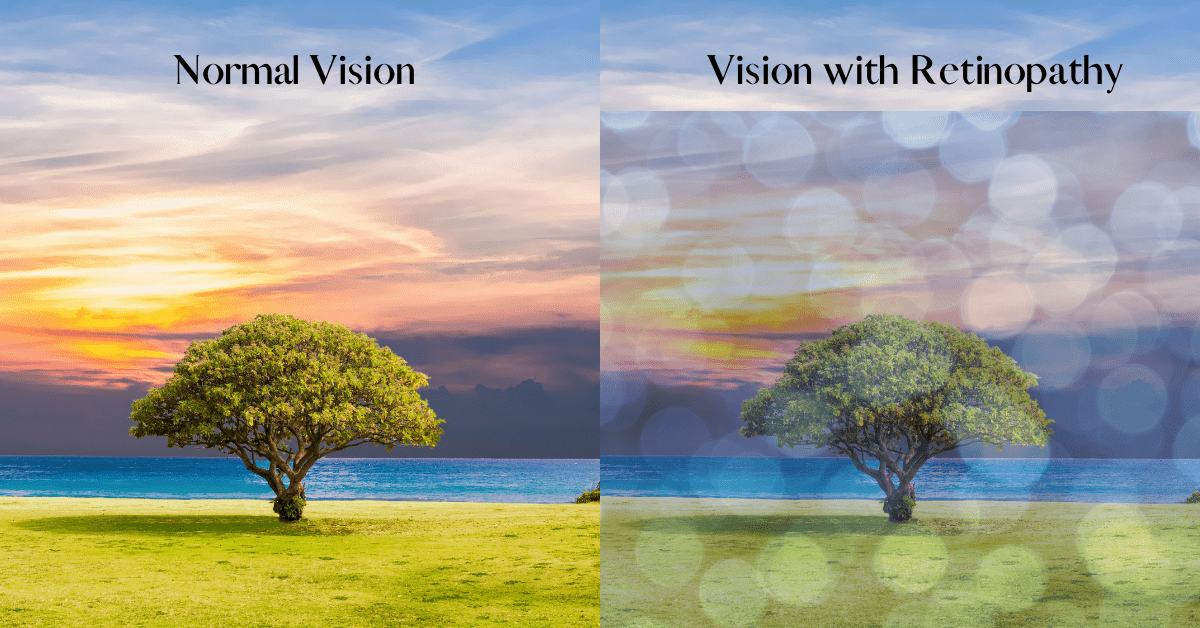
Diabetic retinopathy is called when diabetes affects the small blood vessels in the retina, the part of the eye that acts like a film in a camera. The affected blood vessels become leaky and start secreting fluid and blood into the retina.
Diabetic retinopathy progresses with time but may not cause symptoms until it is quite advanced and close to affecting a person’s sight.
Early detection and timely treatment of diabetic eye disease significantly reduces the risk of vision loss. Since only an ophthalmologist can detect early signs of diabetic retinopathy, all diabetics should have a retinal examination at least once a year.
What Who is at Risk?
All people with diabetes are at some risk of getting diabetic retinopathy, whether diabetes is controlled by diet, tablets or insulin.
You are at greater risk it’s you:
· Have had diabetes for a long time
· Have poorly controlled diabetes
· Have high blood pressure
What How does diabetes affect the eye?
Diabetes results in the weakening of blood vessels in the body which normally supply the oxygen to the retina and thus keep it alive. The tiny delicate retinal blood vessels are particularly susceptible and weakening of these retinal blood vessels leads to leakage or close down. If leakage occurs in Central part of retina called macula, it leads to vision loss. Closure of blood vessel leads to starvation of retina and formation of abnormal blood vessels which are fragile and pose a constant rate of bleeding at any time and leading to severe sight threatening complications.
What are the tests that need to be undertaken for diabetic retinopathy?
Ophthalmoscopy:
Provides a magnified view of the eye structures in detail, enabling diagnosis to be made for a variety of eye conditions. A special magnifying lens is used to examine the retina.
Fundus fluorescein angiography (FFA):
This test involves injection of a dye into the blood and photographing the retina with blue light. It helps to detect abnormal leaky blood vessels which need treatment.
Optical Coherence Tomography (OCT):
Optical coherence tomography is a technique for obtaining cross sectional images of retina especially the important macula area, which is often swollen in diabetes.
What are the treatment madalities?
Laser photocoagulation:
The purpose of the treatment is to arrest progress of the changes within the retina and help to retain existing vision.
Photocoagulation helps regression of abnormal new blood vessels, thereby reducing the chances of vitreous hemorrhage( bleeding) and retinal detachment.
Intravitreal injections:
Certain inject-able drugs called anti-VEGF (Example –Razumab INJ, Accentrix INJ & Eylea INJ) will help to eliminate Leaky blood vessels from the retina. Sometimes steroid injections may also be needed to reduce leakage of fluid into the retina.
Surgery:
VITRECTOMY for removal of vitreous (gel) of the eye may be necessary in advanced cases.
What Remember:
1. Diabetes is a common cause of blindness.
2. In case if you are a diabetic for more than 10 years there is a fair chance that you might have developed diabetic retinopathy.
3. You might have developed the diabetic retinopathy in spite of good vision.
4. Early detection and treatment save the eye.
5. You should keep your blood sugar levels under control.

Glaucoma Treatment
What is Glaucoma?
Glaucoma is a progressive optic neuropathy. It is a damaged caused to the optic nerve due to increase in intraocular pressure or deficit blood supply. The chronic variety of this disease is like a slow poison. People seldom notice the symptoms until considerable nerve damage has occurred. Once damage has occurred, it cannot be reversed. Optic nerve damage causes loss of visual acuity as also field of vision. Health the important aspect is the early diagnosis and prevention of progression of the disease.
What causes Glaucoma & How does if affect the eyes?
In a normal eye there is a continuous circulation of fluid cal aqueous humor, which is secreted by structure call ciliary body positioned behind the colored portion of eye known as iris. This fluid passes through the central opening, pupil and into the spaces called anterior chamber. This fluid then drains into the structure called trabecular meshwork and into the veins. Aqueous humor is responsible for the nourishment of vital structures as also its pressure helps in maintaining the shape of the eye. This pressure is called Intra ocular pressure (IOP). This pressure can rise either when the secretion of aqueous increases as a inflammation when the drainage gets blocked. Increased IOP puts pressure on the optic nerve and creates a cup on a surface. This can also block the small vessels in the nerve leading to ischemia and resultant nerve damage. Alternately if the blood vessel to the optic nerve is compromised, there can be optic nerve damage even if the IOP is normal.
Glaucoma Generally is of Four varieties:
A) Congenital Glaucoma: this action call buphthalmos occurs in newborn children and is characterized by abnormally large and cloudy Eyes and it has to be treated surgically.
B) Chronic Glaucoma: this is the most common variety. Optic nerve damage can occur if the IOP is higher than what the eye can tolerate. The normal range is about 14 to 20 mm Hg. However this is relative and various individually
C) Acute Glaucoma: this constitutes medical emergency. The patient develops is sudden blurring of vision with severe pain around the eye and main also associated with vomiting. Permanent damage can occur in a matter of few days.
D) Secondary Glaucoma: this occurs as a side effect of some other diseases like bleeding, inflammation, tumor, hyper mature cataract etc
Anatomical there are two types of Glaucoma:
· Open angle glaucoma where there is no obstruction to the fluid flow but the drainage pores are blocked
· Closed angle glaucoma when the fluid flow is obstructed from reaching the drainage area by iris bulging forwards.
What are the symptoms of Glaucoma?
Generally symptoms are noticed in conditions of acute angle closure glaucoma. The patient gets severe pain around the eye associated with headache vomiting and occasional dehydration. There is a blurring of vision. The eye becomes congested and the patient complains of saying colored halos around the light.
In a chronic type, symptoms like tense feeling and recurrent pain around Eyes, frequent changes in refraction (change of glasses prescription especially for near vision) and rainbow colored haloes around light if seen should alert you to seek a medication opinion. Subsequently, the patient notices constriction of visual fields when considerable damage has occurred.
Who are at risk? Who should undergo screening test?
Glaucoma can be present at work or may develop latter as Juvenile or developmental glaucoma. However all adults over the age of 35 years, with the presence of any of the following risk factors should get a screening test done for glaucoma
Risk factors:
• Family history
• Diabetics/Hypertension
• Long term corticosteroid use.
• Injury to the eye.
• Elevated IOP
• Myopia
• Thyroid disorders
* If you are over 35 and say yes to any of the above, you have to get screening test for glaucoma.
Diagnosis of Glaucoma:
Many of times, glaucoma is detected during routine eye examinations. When you go for an eye check, it is important for the doctor to know about your
daily medications, family history of glaucoma & general ailments like diabetes, hypertension, thyroid disorders etc.
A) Examination of optic nerve: During the course of routine eye check, examination of optic disc gives an initial clue about the disease. However this has to be confirmed by stereo examination of the optic disc.
B) Documentation of optic disc: the status of the optic nerve at the stage of diagnosis should then be documented with fundus photography which is vital for follow up of the disease.
C) Visual fields: the structural optic disc defect is then correlated with the functional changes recorded by doing visual field examination. A positive correlation only can establish the diagnosis
D) IOP: intraocular pressure help in establishing the intensity of the disease and act as a marker of its control. Intraocular pressure is recorded as a single modifiable risk factors in controlling glaucoma. After a detailed work up, your doctor decide an ideal target IOP customized for you to maintain. Generally it is in range of 12 to 20 mm HG.
E) Gonioscopy: this is a very important investigation that helps to know about the type of glaucoma. The management varies for angle closure and open angle glaucoma and the gonioscopy helps in establishing this fact.
F) OCT: this advanced Diagnostic tool is called optical coherence tomography, commonly known as eye scan. This gives a lot of metal information of the thickness of retinal nerve fibre layer and structural defect of the optic nerve head. This instrument is also used to measure the corneal thickness which is useful to assess the target pressure desired for each patient at every stage.
G) Structural and functional correlation: To conclusively diagnose glaucoma we have to clinically correlate structural defect as detected by optics disc exam/ photo and OCT with the functional defect as determine the visual fields.
Treatment:
There are essentially Three Types of treatment for the control of glaucoma. All are aimed at reducing the IOP to the targeted level.
A) Medical: there are different medications for the control of this disease. Your doctor has to decide the best one for you taking into the consideration its mechanism of action, side effects and your compliance issues as also the cost. Generally the medications needs to be taken lifelong.
B) Laser treatment: two types of laser have a role. YAG laser done to create an opening in the Iris to overcome the blockage of the fluid in case of angle closure(laser iridotomy). Argon laser can be used to increase the flow of fluid toward the drainage area( laser trabeculoplasty).
C) Surgery: In event of both Medical and Laser options being ineffective, surgery may be required. The commonest surgical procedure done is trabeculectomy.
Instruction to the patients:
- Use your medications regularly. Make your medication a part of your daily routine. You may forget a meal but please use your medication as per schedule. Fluctuations of IOP resultant due to poor compliance is bad and promotes progression of the disease. If you forget a dose, take it immediately when you remember and not wait for the next schedule.
- Your doctor is half of the treatment team. You are the other. When your doctor is your primary resource, you need to work with him to protect your vision. Compliance is the key.
- Stays informed and know your medication full. It is recommended that it you understand your disease and also informed about the basic mechanism of action good and side effects of you are using.
- Pay attention to how you are eyes feel and look. Watch out for any unusual changes and report immediately. Do not stop medication without consulting your doctor. The symptoms to watch out for are excessive irritation, itching, floaters, flashes of light, blurring of vision, congestion, discharge and headaches.
- If you are in control, don’t let glaucoma limit your life. Barring a little requirement of medication there is nothing to stop you from leading a normal life. Develop a positive attitude to life.
- Regular exercises result in in keeping glaucoma under control. It also has a beneficial effect on control of risk factors associated with glaucoma.
Remember:
- Glaucoma is not curable but it can be properly controlled by medication
- If it is left untreated it may result in total blindness.
- About 10% of patients may still have progression of loss of of vision in spite of proper treatment.
- Regular checkups with your doctor goes a long way in keeping your disease in check.
- Consider glaucoma not just as a disease but as a way of life and be positive.
Facilities at Swarup Eye Centre:
Swarup Eye Centre offers a comprehensive glaucoma workup and scientific management if diagnosed positive. We have all the equipment needed for a comprehensive work up. The department of glaucoma is headed by Dr. Manoj Chandra Mathur who has to his credit considerable experience in this field.

Pediatrics & Strabismus
Myopia– A Global Pandemic
What is Myopia ?
Myopia, also called near sightedness, is a condition of the eyes, wherein the patient has a good near vision but faces a difficulty seeing things from afar.
Prevalence of Myopia
Myopia is becoming increasingly prevalent around the world, with a recent study showing that close to 30% of the world’s population is currently myopic. Alarmingly, by 2050, close to 50% of the global population will be myopic.
Myopia How is a mypoic eye different from a normal eye?
Myopia is a condition wherein the eyeball is elongated or too long. However, it can also be caused by the cornea(front cover of the eye) and/or lens being too curved for the eyeball length. Some cases of myopia are due to a combination of these errors.
Due to this, the light rays entering the myopic eye from distance get focused in front of, instead of at the back of the eye i.e, on the retina.
Myopia What causes myopia?
The exact cause is not known. Factors that might lead to the development of myopia are heredity, excessive reading, excessive screen time, overuse of computers and gadgets, intensely close visual work, cataracts, health conditions such as diabetes, etc.
Myopia What are the types of Myopia?
Myopia can be
- Congenital, wherein, the child is born with myopia
- Developmental/School myopia, that’s usually not associated with other eye abnormalities. Commonly seen in school going children and gets stabilized by teenage.
- Degenerative/Pathological, that rapidly progresses, and is usually associated with other eye
abnormalities.
Myopia How do i know i have Myopia ?
You are likely to be a myope if you experience the following:
- Clear near vision and blurry distant vision, i.e, you can read from a book clearly but you face a problem driving, or while watching TV or while reading the sign boards. A child might complain of not being able to see what’s written on the black board or he/she might watch TV sitting very close to it.
- Squinting or partial closing of the eyes in order to see clearly.
- Headaches mostly related to eye strain.
- Frequent eye rubbing.
- Frequent eyelid swellings
Myopia What are the risks associated with Myopia ?
Uncorrected myopia can lead to irreversible blindness called amblyopia or lazy eye. Degenerative myopia can eventually lead to many sight threatening complications like glaucoma, cataracts and retinal detachment and macular degeneration.
Burden of myopia:
Myopia is now a global problem, becoming increasingly prevalent at an alarming rate around the world. A recent study shows that close to 30% of the world’s population is currently myopic. Alarmingly, by 2050, close to 50% of the global population will be myopic. We, at Swarup Eye Center, strive hard to prevent you from landing on the bad side of this statistic!!! In addition to the direct economic and social burdens, associated ocular complications may lead to substantial vision loss.
Myopia Management of Myopia
Step 1
Detection of myopia:
An annual checkup of all kids helps detect this condition. Myopia is accurately diagnosed by a cycloplegic refraction i.e, assessing the amount of myopia after putting cycloplegic eye drops.
We, the Swarup Eye Center also conduct screening camps at many schools for this purpose.
Step 2
Once detected, it needs to be corrected and controlled from progressing further and fast.
Myopia Control
Several modes of control are in vogue. Some of those that we provide to our patients are
1) Lifestyle Modification: As many environmental and lifestyle related factors are being studied as causative factors for myopia, some modifications are proving to be beneficial.
2) Encouraging outdoor activity : Studies have shown the protective effect of outdoor activities in reducing myopic onset and progression in schoolchildren.
3) Reduction of screen time or near-vision work has also been shown to be of help.
Remember the 20/20/20 rule – focus on something 20 feet away for 20 seconds every 20 minutes). Holding books or devices close to the eyes needs to be avoided.
- Diluted Atropine 0.01% eye drops: We have been prescribing these eye drops that have been consistently showing promising results by halting or slowing the progression of myopia. These act by preventing the elongation of the eyeball. These are commonly used in the age group between 3-16 years of age. Ex : Myatro eye drops, Myostop eye drops.
- Orthokeratology / Corneal reshaping: It involves use of a special type of contact lenses (rigid, gas-permeable lenses). When worn overnight, these devices reshape the cornea and provide transient (36 to 48 hour) relief from myopic refractive error. Furthermore, RGPs reduce axial eyeball growth, thereby reducing myopia progression.
Myopia Correction:
There are various ways to correct myopia
- Spectacles (concave lenses)
- Contact lenses
- Orthokeratology
- Surgical treatment
SECTACLES
Concave lenses are prescribed in the form of spectacle frames. These lenses bend the light entering the eye in a way that they are focused accurately onto the retina. Strong prescriptions create distortions such as prismatic movement and chromatic aberrations.
CONTACT LENSES
These are an efficient alternative to spectacles. Also, they give a better quality of vision. Many different types of materials are available with us. Many different regimes of wear are prescribed according to the patient’s needs. Strong prescriptions of contact lenses, unlike the spectacles, do not cause distortions.
SURGICAL MANAGEMENT/ REFRACTIVE SURGERY:
Refractive surgery is the term used to describe surgical procedures that correct common vision problems (myopia, hypermetropia, astigmatism and presbyopia), hence reducing or eliminating your dependence on spectacles and contact lenses.
The refractive surgeries we provide are
A. LASER assisted surgeries:
A unique beam of laser is used to scrape tissue without affecting the underlying and surrounding tissue. This makes it ideal for changing the shape of the cornea, the front window of the eye, to reduce or eliminate focusing problems.
1. Blade LASERS LASIK:
An instrument called the microkeratome is used to painlessly remove the outermost layer of the cornea (called epithelium) usually after being loosened with a dilute alcohol solution in the area that will receive laser treatment. This exposes the inner cornea which the computer assisted laser will begin to re-sculpt the curvature of the eye.
2. Blade free LASERS (only LASEK)
A. PRK:
The thin outer layer of the cornea (epithelium) is removed and discarded with an alcohol solution and a surgical instrument, prior to reshaping the underlying corneal tissue with an excimer laser.
B. Trans PRK with Smart Surf Technology:
Treatment is done without touching the cornea and the accuracy of treatment is excellent. It requires no flap creation and is very comfortable for the patient. Using the laser, the epithelium (the outer surface of the eye) is gently removed and the cornea precisely reshaped.
Ex : Schwind SmartSurf
C. Bladeless LASIK:
Also called blade-free LASIK, all-laser LASIK, or femto LASIK. The microkeratome/blade is not used. The surgeon uses two types of lasers for the vision correction procedure. First, a femtosecond laser creates a thin flap in the cornea. Next, the excimer laser reshapes the underlying cornea.
Ex: Intralase
D. Non LASER Surgeries Phakic Intraocular Lens:
Implantable lenses are another surgical option for correcting myopia, particularly for patients with high myopia or thinner-than-normal corneas who aren’t ideal candidates for LASER procedures. These are like contact lenses, but are surgically and permanently placed within the eye and are permanent.
Clear Lens Extraction
This is another viable option wherein the lens, even without a cataract can be removed and a suitable intraocular lens can accordingly be placed inside the lens bag.
We, at Swarup Eye Center, are well equipped and updated and hence, we try our best to be provide our patients with the latest, effective and customized treatment to prevent, treat and control myopia.
Hence, we strive to make sure our patient enjoys the best quality of Vision.
You can help the world fight this pandemic of modernity by following this information brochure.

Lasik & Refractive Surgery
Lasik(Laser-assisted in situ keratomileusis) is a commonly practiced procedure to correct the refractive power of the eye. It is one of the best alternatives to spectacles and contact lenses which is approved by FDA. Lasik is generally considered safe, relatively painless with fast recovery and with less than 1% of post-operative complications.
Eligibility of Lasik:
- Patients above 20 years of age with good corneal thickness, stable refractive power and Normal Systemic health are generally considered good candidates for LASIK surgery.
- Contact Lens users should stop using lenses for 2 weeks prior to LASIK Evaluation.
- Patients with 40 years of age may experience a problem with their near vision (presbyopia) which gradually increases with age. They can opt for monovision correction where the dominant eye is corrected for distance vision while the other eye is corrected for near vision. But patients may take time to get adapted for monovision correction.
Contradications for Lasik :
· If patient is pregnant/ nursing, the changes in vision are due to hormonal changes in the body. So, they can’t undergo surgery.
· Patients with dry eye syndrome should be screened and treated before undergoing LASIK. It may cause severe problems after surgery.
· Patients with relatively large Pupil size, they may experience poor night vision, glare and Hallows after surgery.
· Patients with Keratoconus / other corneal degenerative conditions are not eligible for LASIK.
Procedure How Lasik Works?
In Myopic patient, where the refractive power of the eye is more than what it requires to form a clear image on retina, the cornea is flattened to decrease the overall power of the eye.In Hypertrophic patient, where the refractive power of the eye is less compared to what it requires to form a clear image on retina, the cornea is steepened to increase the overall power of the eye.
In Astigmatic patient, where the refractive power of the eye is different in different meridians, the corneal curvature is changed in a way to form clear image on retina.
Procedure Is Lasik Permanent?
YES, BUT WITH SOME EXCEPTIONS.
If the vision is stable, patient will be comfortable for around 10-15 years. But once patient reaches 40 years of age, they may need reading glasses which gradually increase with age.
Procedure of LASIK
Blade-Free ReLeX SMILE
- Latest patented advanced flap-free Single LASER technology from Zeiss
- Quick healing and painless post-operative course resum.
- Patented lenticule extraction technology – improved corneal strength and lesser post safety and lesser post operative complications.
- Procedure time: 15 mins per eye.
It includes Preoperative evaluation of eye, Creating corneal flap and Reshaping the cornea with laser to correct the refractive power of the eye.. Preoperative evaluation includes refraction measurement, corneal shape and thickness of evaluation Pupil size etc..
Preoperative evaluation takes roughly around 90 minutes. After preoperative evaluation, surgery takes around 30 minutes with no/minimal post-operative discomfort.
- Before the surgery, numbing drops are placed in the eyes.
- Surgeon will use lid speculum to hold the eyelids open during the surgery.
- Now, suction ring is placed on the eye which prevents the eye from moving during surgery.
- Surgeon will make a flap on cornea using blade or laser.
- Once the flap is gently folded back, Surgeon will precisely remove the tissue on the cornea to change the corneal curvature and its power.
- Now the flap is placed back into its original position
Recovery time after LASIK surgery varies by patient, depending on several factors. Typically it takes around 6 – 12 hours. Some patients may take a week for full recovery. Generally it is safe to take rest for 24 hours after surgery without straining the eyes.
Alternatives for LASIK
Even if a patient is not eligible for LASIK, there are many alternatives like
Customized FEMTO-LASIK
o Blade-free flap created using Visumax Femtosecond LASER followed by Corneal reshaping using the Schwnd Amaris laser platform.
- Time tested 2-LASER LASIK technology perfected over 3 decades.
- Quick healing and relatively painless past-operative course.
- Procedure time: 20 min per eye.
Photorefractive keratectomy (PRK)/ Trans PRK –
o Flap free patented advances single-step SMARTSURF surface laser technology.
o Slower healing over 2-3- weeks.
o Mild post-operative discomfort for 3-4 days.
o German Schwind AMARIS laser platform.
o Procedure time 10 mints per eye.